Here are some shortened, subtitled sections of our Making It Easy video.
Introduction (Making It Easy – v1.12)
Unclear terminology (Making It Easy – v2.12)
Teach back (Making It Easy – v3.12)
Here are some shortened, subtitled sections of our Making It Easy video.
Introduction (Making It Easy – v1.12)
Unclear terminology (Making It Easy – v2.12)
Teach back (Making It Easy – v3.12)
Health Literacy in Scotland: Making it Easy
See the subtitled version here.
Why must we make it easy? It has been found that people remember and understand less than half of the information that we discuss with them, also you can’t tell who has understood by simply looking at them.
Improving people’s understanding is crucial for improving patient safety, communication, effectiveness, self management and health literacy.
The Patient Rights (Scotland) Act 2011 states that people should be communicated with in a way that they can understand and that healthcare staff should make sure the patient has understood the information given.
To make it easier we have split our making it easy video into smaller chunks. The full video is at the bottom of the page.
Health Literacy In Scotland – Making it Easy (introduction)
Making it Easy – Section One Health Literacy – a hidden problem
Making it Easy – Section Two Health Literacy – the impact
Making it Easy – Section Three Health Literacy – how can we make it easy?
Full Video
Our latest blog to mark Health Literacy Month 2020 is from Susie Ferguson. Susie is a Disability Employment Advisor with the Department of Work and Pensions. In her blog Susie talks about working in partnership with the Public Health Improvement Team to organise health literacy training for her DWP colleagues.
Part of my role as a Department for Work and Pensions (DWP) Disability Employment Advisor is making sure frontline colleagues are equipped with the appropriate skills and knowledge to support vulnerable clients and people with complex needs, health issues and disabilities.
After working alongside the Community Mental Health Team for four years as an Individual Placement and Support worker, I approached the Public Health Improvement Team to ask how we could further support our public: they embraced the request and we set up small focused groups to discuss the way forward. The Public Health Improvement officers spent time in various Jobcentres, shadowing colleagues in different departments and getting a real feel for what challenges front line staff face on a daily basis.
We settled on 4 main areas of support that would be beneficial to Jobcentre staff and one of those was around health literacy. The Health Literacy Training gave staff the knowledge and confidence when having difficult conversations, and being able to empower people to self-manage and maintain good health.
Despite COVID-19, the Health Improvement officers, Eileen and Morag, were swift to make contact and offer a virtual experience for us. They understood that during this time it was even more important that we were ‘armed with the correct tools’ to be able to offer ongoing support to our vulnerable customers. The training was definitely tailored to our job roles, and in particular highlighted some excellent tips on handling difficult conversations.
I feel that the training has definitely increased my knowledge of what health literacy is and why it is important, and I feel better equipped and aware of the resources and information available, and where to find them. I am much more confident that I can provide the right support to our customers to have improved health literacy.
NHS Scotland have launched a public campaign to support patients and health and care professionals to have positive conversations about care and treatment.
The key message of the campaign is that it’s okay to ask questions of health and care professionals. NHS Scotland have suggested four key questions for patients to ask:

We know that when patients have a better understanding of their health, and of the treatment and care options that are available to them, they can make more informed decisions about the care that is right for them. It is also very important that professionals support and promote conversations that encourage shared decision making.
For further information about the campaign, including a range of resources for both patients and professionals, please visit NHS Inform.
The “It’s OK to Ask” campaign was developed and piloted by NHS24, and received support from the Realistic Medicine Value Improvement Fund.
Everyone in Scotland should now have received an invite for their first COVID-19 vaccination appointment.
However, many have still to come forward for their vaccine. It’s really important that all those eligible come forward as soon as possible and get both doses of the vaccine to ensure maximum protection from COVID-19 and help us win the race against the virus.
Please help us to encourage people to take up the vaccine by:
You can download all campaign materials from the COVID-19 VACCINE DROPBOX and you can also view the Vaccinations Toolkit leaflet which includes links to further information.
Key Messages
Core
Safety
Side Effects
Pregnancy and Breastfeeding
Fertility
For more information about the campaign please contact health@smarts.agency
Our closing blog to mark Health Literacy Month 2020 is a video from Dr Gregor Smith, Chief Medical Officer for Scotland. In his blog he talks about the importance of health literacy particularly with regard to our response to the Covid-19 pandemic.
Health Literacy Month – Dr Gregor Smith from Alan Davidson on Vimeo.
Dr Kate Arrow, Scottish Clinical Leadership Fellow and Anaesthetic Specialty Registrar in NHS Tayside blogs about improving access and experience for patients.
Think about the last time you bought something? Maybe an item from an online shop? Think about how easy it was?
Online retailers make it almost impossible not to buy their products, ‘popping’ it up in front of you every time you open social media, offering close alternatives, one click purchases and easy returns.
In private industry, the user interface i.e. the way a customer interacts with a service, is vital to sustaining business. Drawing you in and creating the best experience means customers often feel satisfied, loyal and valued.
Now think about an experience of visiting the Doctor or Nurse? Was it as easy?
Public services such as the NHS are working to make it easier to access the information and services that patients need.
Traditionally, services such as health and social care are designed by the people who provide them, often assuming what the patient wants or needs. Services are not consistently designed in partnership with patient and carers, and this can mean that their needs are not met.
Working with patients to design services not only reduces waste and improves experience, it also generates ideas for change.
In NHS Tayside around 2500 outpatient’s appointments are missed each week. At a cost of £151 per appointment, this amounts to around £300000 per week.
On the weekend of 11th & 12th May 2019 a Co-Design Pop Up shop was opened in Dundee Overgate Shopping Centre. It asked visitors to share their experiences of attending NHS appointments by asking the question;
NHS Appointments; What matters to you?
The Pop Up took place during Dundee Design Month and was the first healthcare pop up to feature in the festival of design.
The collaboration between NHS Tayside and Dundee City Council was designed to be visual, interactive, portable, low cost and recyclable.

The focus was;
Reflecting the priorities of Realistic Medicine, “The What Matters to You Campaign” and “Getting it Right first Time”, the shop allowed visitors to follow the patient journey, engaging with touch points to share experiences and generate ideas for change.
Touch Points for this question were;

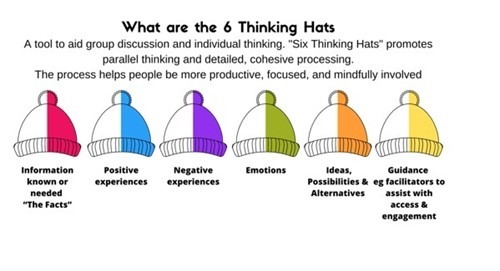
 Medical and design students led visitors through the journey, exploring their experiences, challenges and suggested solutions, through the ‘6 thinking hats’. Visitors walked through the Pop Up as if they were following the patient journey.
Medical and design students led visitors through the journey, exploring their experiences, challenges and suggested solutions, through the ‘6 thinking hats’. Visitors walked through the Pop Up as if they were following the patient journey.

The tone of the experience was positive, no- blame and aimed to leave visitors with optimism by finishing with ‘The Tower of Power’ which asked;
Congratulations! Your input and ideas could save NHS Tayside £300,000 per week.
Where would you spend or invest this money?
Over 2 days the pop up had over 1000 interactions with members of the public. Strong themes emerged from the patient journey, these are summarised in the infographic below

These themes were presented to the service design groups within the Transforming Tayside strategy. The feedback was incorporated into the workstreams of these groups and will from part of their strategy going forward.
The process was an important learning event for the students and health professionals who heard the stories of visitors, both positive and negative, and we hope to present many of the ideas for change to Leaders within the local universities as concepts to explore further within their studies.
The use of design tools such as journey mapping and the 6 thinking hats enabled visitors to share a broad experience and explore a diverse range of thoughts; from car parking to staff morale.
Taking service design into the community meant we heard a widely representative voice from our local population. It demonstrated NHS Scotland’s commitment to public partnership and co-design, aiming to improve services and access for all.
In Scotland, 2% of the population use 50% of resources, our challenge is to promote equity in how our services and information are offered and consumed by our citizens. Partnership with our patients is vital in realising this vision of equitable and collective service design and provision.

Scotland’s earliest champion of health literacy was probably a physician working in Roxburghshire, William Buchan, who wrote:
“Medical authors have generally written in a foreign language; and those who were unequal to the task, have even valued themselves upon couching .. their prescriptions, in terms and characters unintelligible to the rest of mankind. It is not to be supposed that men can be sufficiently upon their guard against diseases, who are totally ignorant of their causes.”
This was written in his best-selling “Domestic Medicine” in 1784 at a time when Scotland was one of the most well read nations on earth. An estimated 75% of the population had adequate reading and writing skills. Buchan understood that for mankind to thrive and be “upon their guard against diseases”, medical authors must “de-medicalise” information and use words and letters which people could understand. He eloquently made the link between literacy and living well. This may be one of Scotland’s first references to “health literacy” and “self management”, and although these terms are contentious, there is seldom any doubt about their relevance to health and wellbeing.
For many years, health literacy, however defined, was a specialist interest of professionals who focussed on children and adult literacy and people with communication difficulties; areas which demanded particular skills to ensure information is communicated in simple terms. However, the benefits of giving and receiving information in an easy to understand format became clear as evidence gathered about the importance of communicating safely in the health environment and the significance of differing levels of understanding.
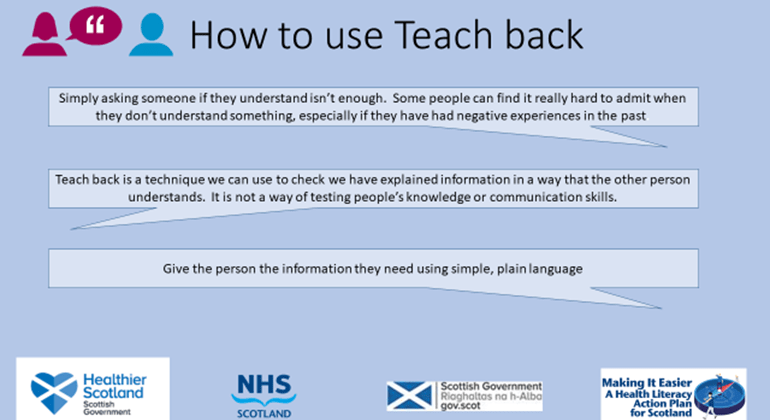
In the early 2000’s, there was a flurry of activity worldwide as papers were published about the benefits of checking understanding and using approaches such as Ask Me 3 and Teach Back .
In 2003, the Institute of Medicine’s report, “Priority Action for National Action in Quality Improvement” , part of the Quality Chasm Series, recommended a set of 20 priority areas for the US Department of Health and Human Services. One of the 20, described as “cross cutting”, was health literacy and self management.
The key link between health literacy and control of conditions such as diabetes was also being made. Clinicians, such as Professor Dean Schillinger, provided evidence that people with inadequate health literacy and type 2 diabetes had worse glycaemic control and higher rates of retinopathy than their peers with adequate literacy.
Interest remained scattered and unconnected across Scotland, as it was in most countries, and activities were not necessarily labelled “health literacy”. However, many adult literacy initiatives, such as The Big Plus, a National Adult Literacy and Numeracy campaign, and Adult Literacies Online , made numerous references to health in their campaigns.
Keep Well, a national plan to address health inequalities in Scotland, contributed useful research about health care staff’s approach to literacy and health in “Exploring Primary Care Responses to Adult Literacy Issues” in NHS Greater Glasgow and Clyde (2008). Conclusions were that some staff were reluctant to raise the issue of literacy and questioned whether they should be addressing literacy issues, which could result in a lost opportunity to signpost people to support.
An important contribution to knowledge about health literacy was made in the UK when Coulter and Ellins’ published a Review of Patient-Focussed interventions (2006) , which included a very useful section on health literacy. This provided an excellent reference when, in 2008, the Health Improvement Strategy division of the Scottish Government commissioned a Health Literacy Scoping Study . This was a major step forward, as this represented an opportunity to gather intelligence and start planning a national approach. The Health Literacy Scoping Study explored the concept of health literacy, its application to policy and practice in Scotland and identified options for further development.
Another impetus was a key finding in the Scottish Survey of Adult Literacies in 2009, which was that: “26.7 per cent of the population may face occasional challenges and constrained opportunities due to their literacy skills. Within this quarter, 3.6 per cent face serious challenges in their literacy practices.” “People with occasional difficulties” referred to the huge number of the citizens of Scotland who manage well in an unchanging environment, but struggle to make sense of an unexpected change in their health, such as being given a diagnosis of a long term condition, being prescribed medicines or being admitted to hospital. This survey confirmed that the unfamiliar health environment remained “unintelligible to the rest of mankind”.
Further momentum was gained when the Scottish Government produced strategic guidance in 2010 in Adult Literacies in Scotland 2020 , which stated ‘Making sense of complex health environments and information can be challenging for us all; however, poor “health literacy” affects a large part of the population.” The guidance recommended that there should be a focus on literacies and health and well-being, and made clear that poor health literacy had equal importance for people working in the health services; “complex health information can also be challenging for some health care staff, who may have to deal with dosage, report writing and communicating with patients in a variety of ways”.
Meantime, directorates in Scottish Government were collaborating to develop the connections between health improvement, self management of long term conditions, functional literacy and patient safety. One outcome of this collaboration was a lively event in March 2010, “Mrs Dalrymple’s Toe” – examining the link between poor literacy and poor health outcomes” when adult learners, professionals from the world of education, literacy, third sector, health and social care and policy makers, gathered to discuss whether there should be a national focus on health literacy, the answer was a resounding “Yes”.
A significant advance was made later in the year, when health literacy was identified as a key component of the person centred ambition in Scottish Government’s Healthcare Quality Strategy for NHSScotland. This focus was provided in 2011, when the Scottish Government appointed a Policy Lead for Health Literacy and a National Clinical Lead for Health Literacy and Self Management. The following year, the National Health Literacy Action Group (NHLAG) was established, chaired by the Chief Executive of the Health and Social Care Alliance Scotland (the ALLIANCE), the national third sector intermediary for a range of health and social care organisations. The remit of the NHLAG was to “provide a national narrative, vision, direction and support to raise awareness and reduce the negative impact of poor health literacy.”
And so now, two hundred and thirty years after William Buchan’s far sighted reflections, Scotland’s first Health Literacy Action Plan is being launched with an ambition to ensure that the people of Scotland have the opportunity to live well and “be sufficiently upon their guard”.
Christine Hoy, Primary Care Development Manager, Health and Social Care Alliance Scotland
Christine has spent much of her career in practice nursing in NHS Lothian. Following a scholarship to study health literacy and self-management internationally, she was seconded to Scottish Government to establish a self-management programme, and retains a keen interest in health literacy.